- Despite widespread assumptions to the contrary there is little evidence that climate change has resulted in an increase in infectious diseases.
- Researchers suggest it is the conditions in which diseases are affected by climate change that is the basis of concern.
- Even those proposing this admit it is a minor effect, and it is clear far more has been and could be done, to reduce disease by other measures unrelated to climate mitigation.
It has long been assumed that higher temperatures cause a rise in the incidence of infectious disease. For example, some arguments claim that global warming will increase the range of mosquitos that carry viruses and parasites (e.g. malaria), and cause food to foul, leading to diarrheal diseases.
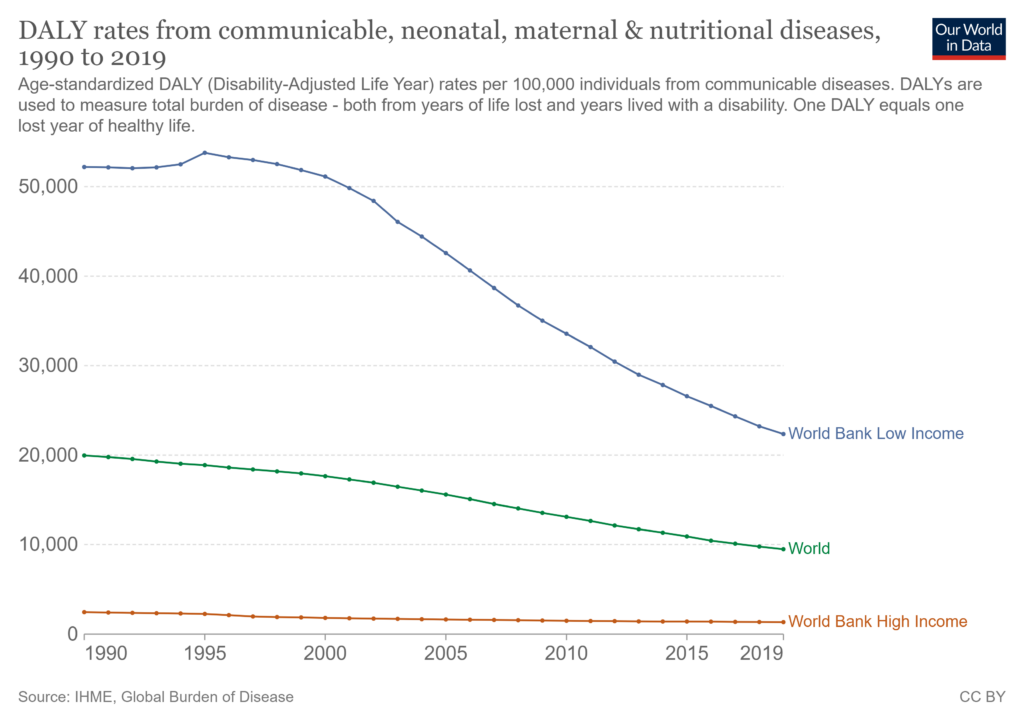
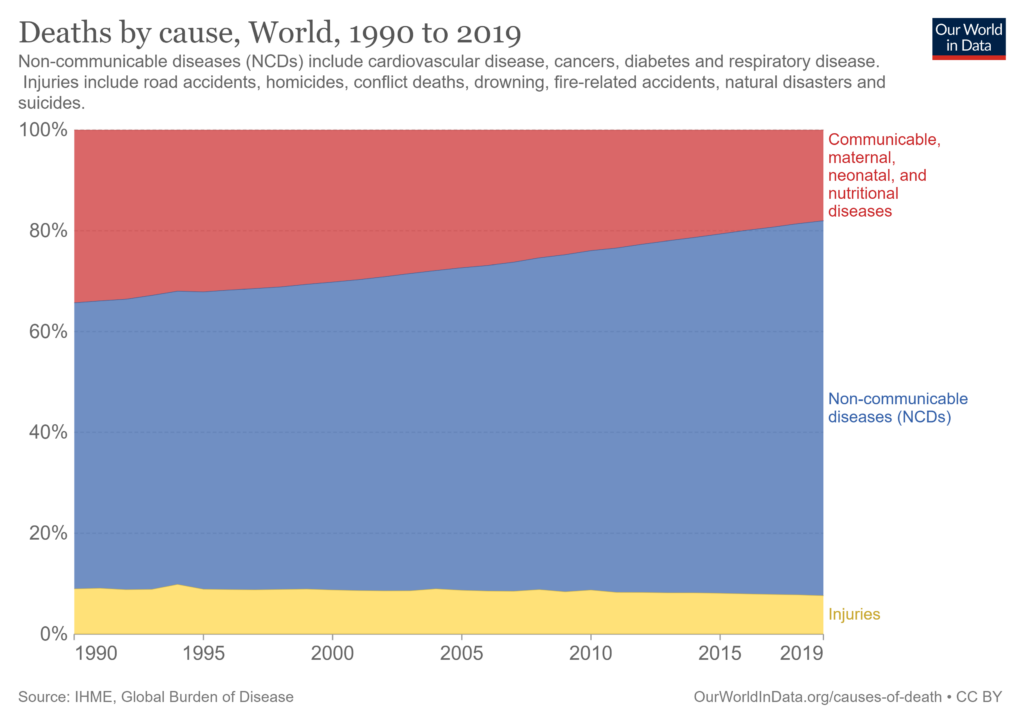
But across the world, even in the poorest regions, the rate of disability-Adjusted Life Years (DALYs) per 100,000 individuals from communicable diseases has fallen significantly since 1990, as has the number of people whose deaths are caused by communicable diseases each year.
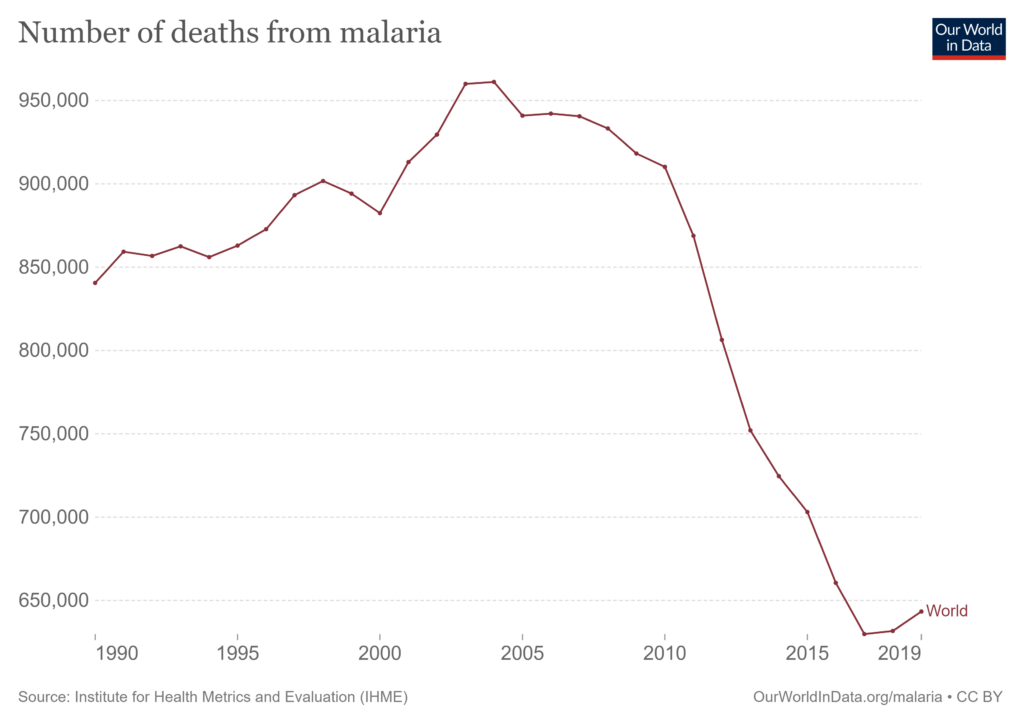
The same is true of malaria, which shows much reduced rates of incidence and mortality.
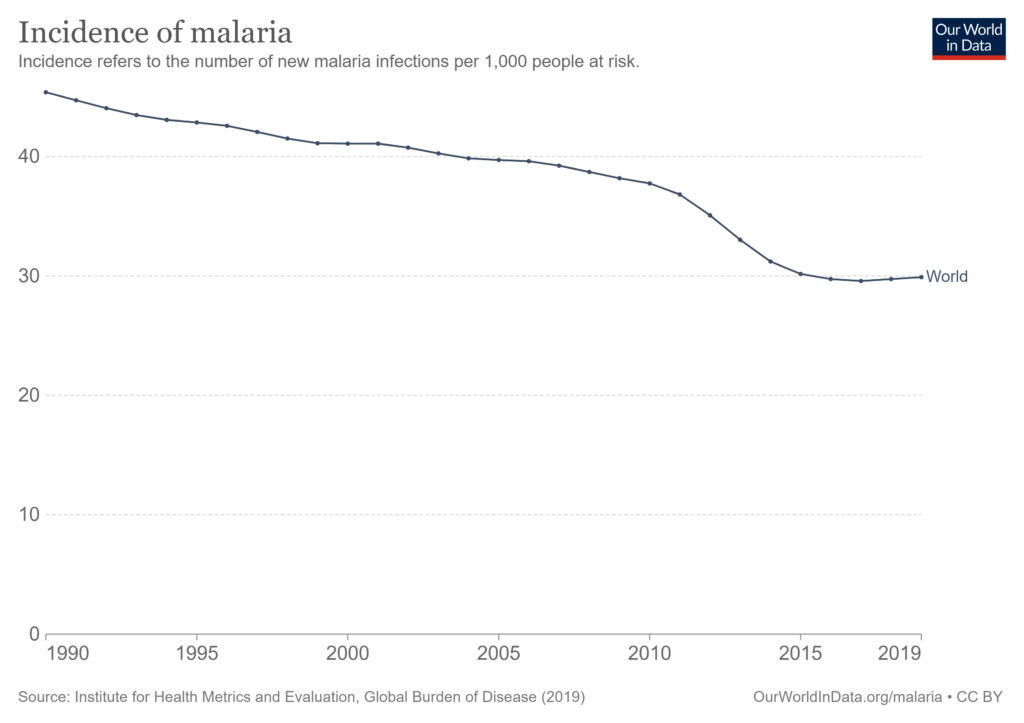
However, some climate and health researchers argue instead that the significant risk factor is not incidence or mortality, but the conditions in which vector-borne diseases are affected by climate change. According to these claims, the range of mosquitos carrying malaria parasites, for example, has increased. One such study, the Lancet’s Countdown on health and climate report claims that ‘the number of months suitable for malaria transmission increased by 39% between 1950–59 and 2010–19 in highland areas of the low [Human Development Index] group’, and that ‘climate change might make malaria eradication efforts increasingly difficult in already disadvantaged areas’, but fails to sufficiently inform readers of the good news depicted in the charts above.
Similarly, though the IPCC’s AR6 WGII notes that malarial rates of transmission and mortality are reduced by ‘non-climatic socio-economic factors’, the progress seen since the turn of the century is all but ignored, and projections of future rates are offered under the assumption of no ‘adaptation’ (i.e. no climate policy). For example, the report attributes ‘high confidence’ to the claim that ‘There is a high likelihood that climate change will contribute to increased distributional range and vectorial capacity of malaria vectors in parts of Sub-Saharan Africa, Asia, and South America’. The report admits that disease models ‘have limited ability to account for population changes and development, investments in health sectors and interventions, and confounders such as age, socioeconomic status, employment and labour migration and climate variability’, but claims nonetheless that ‘available models do allow for projections of malaria transmission under different climate change scenarios to be made with high levels of certainty’.
The report finds that climate change increases the mortality of malaria by 32,700 deaths per year. While this sounds like a significant figure, it omits from the discussion the fact that for each year of the decade to 2017, the annual total number of malaria deaths fell by approximately this amount: from 940,521 to 629,854. The IPCC report seems much more interested in discussing deaths than avoiding them by any other means than climate change mitigation. This is despite evidence of radical reductions in mortality that cannot be explained by climate change, which by the report’s own admission, is a minor effect. Indeed, given the evidence that such remarkable progress in controlling a disease has been demonstrated, one should ask whether there is any significant relationship between climate and malaria, and whether the opportunities for interventions are entirely socio-economic.
These are omissions of good news about malaria from scientific literature and policymaking, and also in research and broader public discussions. Instead of sober reflection, the IPCC’s focus drives alarmist commentary in claims that confuse malaria with other first order consequences of poverty, stating, ‘The global estimates of excess deaths due to malnutrition, malaria, diarrhoea and heat stress are approximately 250,000 deaths per year in 2030-2050 under the medium-high emissions scenario, assuming no adaptation‘.
That is to say that whereas the IPCC devotes much conversation to the ‘co-benefit’ of mitigating climate change (at best saving 32,700 lives from malaria), the IPCC is not distracted by the possibility of saving the remainder of 960,000 lives each year. On the numbers offered by the IPCC itself, malnutrition, malaria, and diarrhoea are each far bigger problems than climate change. From the sceptic’s perspective, then, the IPCC’s treatment of malaria is not merely misleading, but misplaced. Far more good could be done by tackling these far more real and tangible problems in the world directly than by mitigating climate change.
